Cards In This Set
| Front | Back |
|
Hemostasis
|
1. Platelet plug - platelets adhere to collagen @ site of injury --> fibrinogen binds adjacent platelets via GP IIb/IIIa Rs (unstable) = Aggregation
2. Reinforcement of plug (fibrin) = coagulation Fibrin created via coagulation cascade (intrinsic & extrinsic paths) Xa turns Prothrombin --> Thrombin which creates Fibrin Controls: 1) Antithrombin (forms complex with clotting factors, inactivating them Heparin's target 2) Plasmin (digests fibrin) |
|
4 Clotting Factors need Vit K for synthesis
|
VII, IX, X, Prothrombin
|
|
Unfractionated Heparin (UFH)
|
- Enhances Antithrombin activity (neutralizing Xa & Thrombin) --> less fibrin produced --> less coagulation --> hemostasis control
1) UFH + Antithrombin bind --> change in shape of Antithrombin 2) Shape change = increased ability to bind with Xa or Thrombin --> inactivation - NOT orally (must be given parentally via SC, IV) - Variable activity (b/c variable smt Antithrombin) --> must monitor levels via aPTT or Anti-Xa - Antidote = Protamine - Dosing = wt-based, in units (IV if tx MI/DVT; SC if preventing DVT) - For: Rapid anticoagulation (acute MI, PE, DVT, stroke) Prevention of VTE - Hemorrhage = main complication (STOP UFH infusion! Protamine) - Heparin-Induced Thrombocytopenia (HIT) - immune-rxn (Abs + Heparin + platelets bind --> aggregation) Develops 1-2wks after starting therapy (immediately if previous heparin exposure...already have Abs) IVC filter (trap clots) & IV immune globulin (IVIG) - gets rid of clots D/C Heparin! Use alternative anticoagulation agent |
|
Low-Molecular Weight Heparin (LMWH)
|
- Same mechanism as UFH --> but preferentially binds to inactivate Xa (not lrg enough for Thrombin binding)
- More predictable than UFH - No monitoring - Less risk of HIT (safer), also less risk of bleeding Avoid in pts with HIT (cross-reactivity) - SC for both tx & prevention (pre-filled syringes) Good for outpatient setting - Protamine not as effective in countering it |
|
Fondaparinux
|
- Inhibits Xa activity via Antithrombin (same mech) --> less Thrombin --> less Fibrin
- Prevention or Tx of VTE - SC injection once daily (convenient) - No monitoring - X HIT - SE: bleeding |
|
Warfarin
|
- Vitamin K antagonist --> blocks synthesis of 4 factors
Delayed onset (doesn't affect those alrdy created) Not for emergencies Need consistent Vit K intake (don't have to avoid) - For prophylaxis of thrombosis - Intx!! - assume it will interact with any drug - Very little free & thus active (basis for many intx) - Monitor!! Prothrombin Time (PT): detects change in 4 factors International Normalized Ratio (INR) = better - how thin pts blood (normal: 2.0-3.0; high risk: 2.5-3.5) Monitor INR for first 7-10 days, once in range decrease - Orally (IV fastest but risk of anaphylaxis) - no oral form so give injectable stuff orally - PT EDUCATION (signs of bleeding, safety measures to decrease bleeding, inform other HCPs, consistent Vit K, drugs must be approved) - Hemorrhage (screen for high risk, D/C prior to surg) - Vit K can reverse INR - Not during pregnancy or breastfeeding (use Heparin during preg) |
|
New Oral Anticoagulants (Rivaroxaban, Dabigatran)
|
- Less monitoring req'd, No titration, Less interactions
- Expensive (not covered bc limited clinical experience) - Rivaroxaban (inhibitor of Xa) - Dabigatran (inhibitor of Thrombin) - End result of both: less Thrombin --> less Fibrin - Prophylaxis of VTE, stroke |
|
Aspirin
|
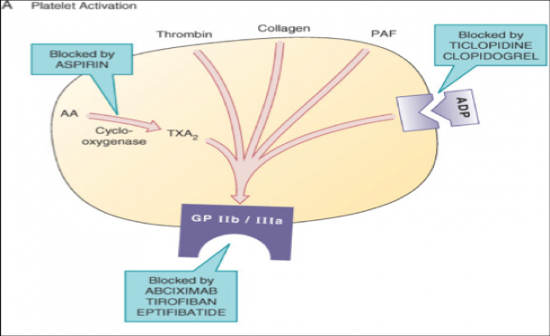 - Irreversibly inhibits COX enzyme --> decreases platelet activation (less binding to GP IIb/IIIa Rs) - Prevention of MI, stroke in those withTIA hx - AEs: increased risk of bleeding, hemorrhagic stroke, GI effects - 81mg Oral --> preventative - 160-325 mg CHEWED --> after acute MI = loading dose |
|
Clopidogrel
|
- Irreversibly blocks ADP R --> prevents platelet aggregation --> preventing coagulation
- Prevention of MI, stroke (in those with hx), during coronary stenting - Well tolerated (GI = minor SE + bleeding) - No Monitoring - PPI blocks conversion of Clopidogrel --> active form --> decreased efficacy of Clopidogrel & increased risk of vascular events |
|
Thrombolytics ("clot busters")
|
- Chews up clots that are already formed
- For acute MI, ischemic stroke, pulmonary embolus - Can only give w/i certain amt of time - SE: bleeding (minimize physical manipulation, invasive procedures, concurrent use of antiplatelet/anticoagulant drugs, monitor potential bleeding sites) |
|
Alteplase (tPA - Tissue Plasminogen Activator)
|
- Increases conversion of Plasminogen --> Plasmin --> gets rid of clots via digestion of Fibrin
- Is a Thrombolytic --> for acute MI, PE, ischemic stroke Low-dose tPA: unblock occluded catheters (Central Venous Catheters) - Expensive!! - CONTRAINDICATIONS! (recent bleed, HTN, etc.) |



