Cards In This Set
| Front | Back |
|
Pericardial sac aka pericardium
|
 Fluid filled outer layer of the heart' provides prtection and reduces friction of heart |
|
Medistinal cavity
|
 Region where heart lies; between left and right lungs |
|
Heart wall has 3 layers: name them
|
 1. epicardium: inner layer of pericardium 2. myocardium: middle layer of heart muscle: houses cardiac muscle fibers: source of contraction site 3. endocardium: innermost layer of the heart |
|
4 chambers of heart: name the two 2 types and what their general purposes are
|
-atrium: receive blood returning to heart from the blood vessels
-ventricles: pump blood into blood vessels
|
|
Name two types of blood vessels and their general flow of blood
|
-veins: bring blood to the heart
-arteries: bring blood away from heart to other body parts etc
|
|
Right side of the heart: anatomy and functions
|
 -right side of the heart receives deoxygenated blood and sends it to the lungs for oxygenation -superior/inferior cava: veins from upper/lower body bring blood to the right atrium(deoxygenated) -pulmonary circuit: brings blood to lungs from right ventricle, after oxygenated the blood returns to left atrium -low pressure system: only needs enough to get to lungs and back -tricuspid valve: valve between the right atrium and the right ventricle pulmonary semi-lunar valve: prevents back flow into the right ventricle: valve between the right ventricle and the pulmonary artery -pulmonary artery: pumps blood to the lungs via this(artery = away from heart) from right ventricle |
|
Left heart anatomy and functions
|
 Left heart = receives oxygenated blood from lungs and pumps it to rest of body -pulmonary vein: sends O2 rich blood to the left atrium of heart -systemic route: sends blood to rest of body -high pressure system: left ventricle requires strong contractions to pump blood to rest of body -bicuspid valve: valve between left atrium and left ventricle: aka the mitral valve -aortic semilunar valve: valve between the aorta and the left ventricle: prevents back flow into the ventricle aorta: pumps blood to body from left ventricle |
|
Cardiac muscle
|
Striated
intercalated disks = gap junctions
branched fibers
autorhythmicity
|
|
Autorhymicity
|
Its spontaneous depolarization of the heart muscle tissue
|
|
Functional synctium
-purpose/concept
-difference between atria/ventricle autorhymicity
|
-one signal sent = all muscles contract
-thin membranes between cells
-atria: faster autorhymicity(70/min) due to smaller size
-ventricle: slower autorhymicity(20/min) due to larger size
heart functions off this type of synctium
-if contraction synchrony stops = fibrillation = death
|
|
2 types of cardiac muscle fibers that are involed in depolarization
|
Fast response
slow response
|
|
Fast response fibers
-Na+ gates
-phases(5)
|
 -involve atria and ventricles -potential = -90 to +30mV -2 Na+ channels -1. M gates: activation gates(depolarize) Na+ entry -2. H gates: inactivation gates(repolarize) no Na+ entry -phase 0: depolarization, Na+ influx(fast) -tetrodotoxin = strong inhibitor of channels -phase 1: Na+ channels close, peak of graph(initial repolarization), partial K+ efflux -phase 2: plateau due to Ca2+ influx(slow) and K+ efflux match one another -phase 3: K+ efflux(big), Ca2+ close, repolarization -phase 4: stabilize membrane/resting potential of -90mV |
|
Importance of extended plateau with phase 2
|
-prevents another AP from firing while heart muscle is still contracted
-prevents tetanus of the heart muscle by allowing the contraction/relaxation of the heart to cease as soon as the refractory period is over
ERP = effective refractory period = cant fire an AP while heart muscle is 'contracted' includes phases 1-3
RRF = relative refractory period = capable of firing an AP but must be larger than normal and occurs during the relaxation of the heart muscle
|
|
Slow responses
-phases(3)
|
 -conduction system of the heart -modified cardiac muscle tissue -involve the SA/AV nodes -susceptible to cardiac aschemia -resting potential = -70 to 10mV -unstable membrane potential = wants to depolarize -NO plateau -slow depolarization 'pacemaker' tissue -block potential in slow tissue = signal migfht not get through to heart = heart block -phase 0: slow depolarization(Ca2+ in) -Na+ not as effective -no tetrodotoxin effect here -some K+ efflux -not sharp increase in graph compared to fast response -phase 2/3: repolarization phase(K+ efflux) -Ca2+ close -NO plateau!!! -phase 4: resting potential -leaky channels Ca2+ influx >> K+ efflux -leads to desire to be depolarized -na+ channel influx is low |
|
Conduction system of heart
-nodes
-fibers etc
|
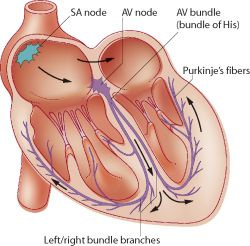 -modified cardiac muscle -SA node: sinoatrial node -autorhythmic cells in right atrium -main pacemaker for the heart -depolarization starts here -fast beat (70/min) -AV node: atrioventricular node -slower beat(35-50/min) -autorhythmic cells near bottom of right atrium -send signals to bundle of His -bundle of His: signal sent to left and right branch bundles -send signal to purkinje fibers -purkinje fibers: specialized conducting cells -contract ventricles of heart upwards from the bottom |



